The 3rd International Congress on Far-UVC Science and Technology (ICFUST) was held in Boulder, Colorado last month, where we had the opportunity to step back from the technical nuances and ask one of the most important questions facing the far-UVC community: How do we move from promise to impact?
We presented our perspective on the far-UVC field, and our focus on its potential to reduce airborne disease transmission at a scale relevant to pandemic prevention. We discussed why this technology excites us, and outlined our vision for advancing research, fostering collaboration, and bridging the gap between innovation and real-world application. We also outlined the role we aim to play in accelerating progress, from supporting critical studies to advocating for deployment strategies that maximize impact.
At ICFUST, we presented our analysis of what's slowing down far-UVC from widespread deployment. The core challenge? We simply don't know how much far-UVC we need to effectively suppress airborne transmission in real-world settings.
How Much Far-UVC Is Enough?
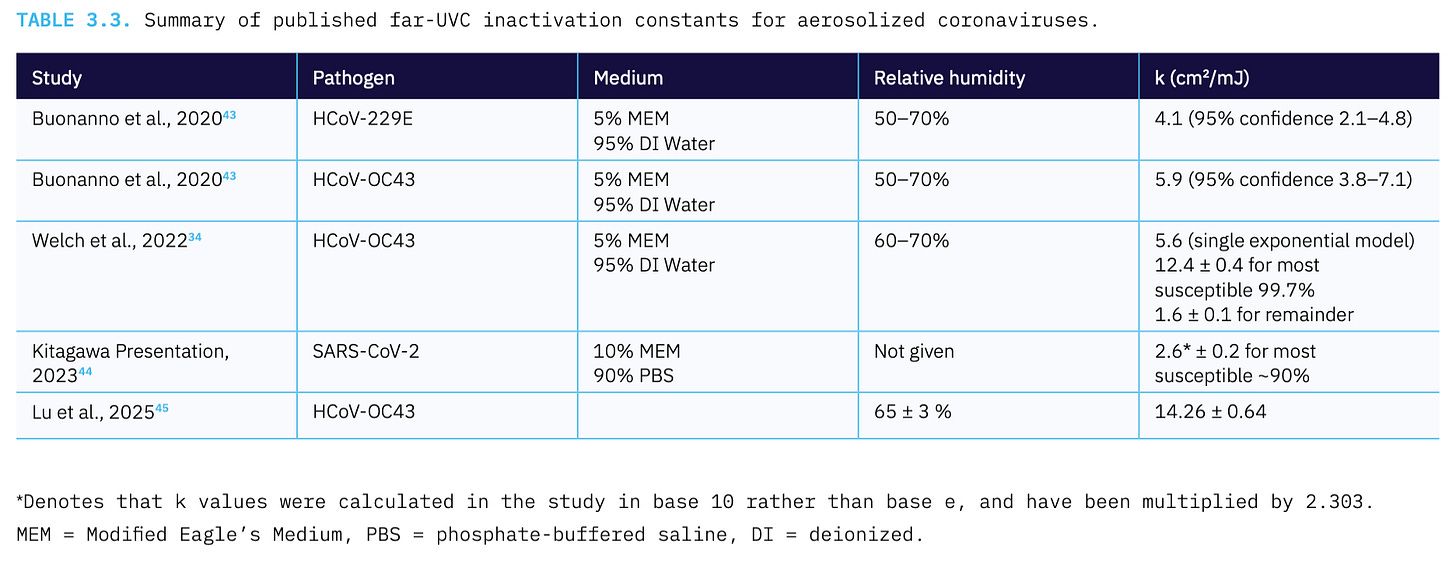
The uncertainty around how much far-UVC is enough to effectively clean the air of pathogens matters enormously. The Clean Air Delivery Rate (CADR) of a far-UVC installation depends on three factors in a well mixed space: UV susceptibility of pathogens (k), power output (P), and average photon pathlength (L). Current research shows order-of-magnitude differences in pathogen susceptibility constants, which translates to order-of-magnitude different estimates in how many far-UVC devices you need in a space to meet clean air targets like the CDC 5 eACH target or the building-specific ASHRAE 241 standard (see Table 3.3 below from the Blueprint for Far-UVC).
The effectiveness requirements for far-UVC directly impact implementation considerations. At higher power levels, deployment becomes more complex: costs increase, we must carefully manage exposure to stay within occupational exposure limits, ozone generation requires attention to ventilation and secondary chemistry, regulatory compliance needs thorough planning, and material compatibility requires evaluation. At lower power levels, implementation becomes notably more straightforward: costs decrease substantially, exposure remains well below occupational exposure limits, ozone production is minimal, devices can easily meet existing certification standards like UL 867 or 8802, and potential material interactions are reduced. Many groups have made important strides on getting clearer on this question, and our intent is to build on that foundation. Understanding which scenario applies will help the industry optimize products and deployment strategies for maximum public health benefit.
Our top recommendation from our Blueprint for Far-UVC addresses this fundamental knowledge gap: Establish how far-UVC installations need to be designed to effectively suppress airborne transmission. This requires four critical research components:
First, we must obtain pathogen inactivation data from actual human respiratory aerosols. Modeling suggests that proteins in respiratory droplets could provide significant shielding, particularly for larger aerosols. Current synthetic media don't capture the complex mixture of salts, organic compounds, and proteins found in human respiratory emissions.
Second, we need controlled bioaerosol chamber studies examining how environmental variables like relative humidity affect pathogen susceptibility to far-UVC. Just as conventional germicidal UV effectiveness varies with environmental conditions, far-UVC's performance likely depends on factors we haven't fully characterized. These studies will help us understand whether installations need adjustment for different climates or seasons, and how indoor environmental conditions might enhance or diminish effectiveness.
Third, the field must understand what causes the dramatic variability in experimental results measuring far-UVC efficacy and develop standardized methods. When different labs report susceptibility constants varying by orders of magnitude for the same pathogen, we can't provide reliable deployment guidance.
Finally, we need modeling that takes these factors into account and accurately predicts pathogen inactivation in real settings, and rules of thumb deployment guidance guided by the empirical evidence and modeling.
The path forward requires filling these knowledge gaps systematically. Once we understand the true susceptibility of airborne pathogens to far-UVC in human respiratory aerosols, we can design installations that deliver sufficient dose to render the air safe from pathogens while maintaining safety margins. This evidence will enable the development of clear deployment guidelines, inform cost-benefit analyses, and ultimately support the widespread adoption needed for pandemic prevention.
EXHALE Request for Proposals
EXHALE (EXposure of Human Aerosols to far-UVC Light for pathogen Elimination) is one current example of how we are trying to answer these questions. We need to quantify far-UVC’s impact on viral pathogens contained in actual human respiratory aerosols, not just artificial media, in order to validate our lab methods against the real thing.
If you have the ideas, the expertise, or the appetite to tackle these challenges, consider responding to the EXHALE RFP or reaching out to collaborate on other critical fronts. Here’s the important details:
Initial abstracts are designed to be short descriptions of the main idea, at a maximum of 4 pages.
Abstracts due July 21.
If you know of someone who could be a fit for EXHALE, we are also offering a $200 referral bonus for people who connect us with researchers we would not have otherwise reached and who end up receiving an award from this RFP.




Can you please give an update on what is happening with regulations being changed to add the US FDA & from the US EPA